Глава 13
Идеальный циркадный день
Мои идеальные циркадные дни начинаются с предыдущего вечера, когда я рано завершаю ужин – примерно в 19 часов – и в 22:30 отправляюсь спать. Утром я чувствую себя отдохнувшим и посвежевшим. После плотного завтрака примерно в 8 часов утра я совершаю короткую прогулку быстрым шагом на свежем воздухе, а затем сажусь в машину и еду на работу. Управление автомобилем становится хорошей разминкой для разума, и я вхожу в свой кабинет уже полностью готовым к началу рабочего дня. Примерно в полдень я делаю короткий перерыв на обед и продолжаю работать до 17:00. Затем отправляюсь в тренажерный зал, немного занимаюсь, а потом возвращаюсь домой и ужинаю с семьей. После ужина я посвящаю еще немного времени работе или помогаю дочери с уроками, используя рабочее освещение.
Как вы уже знаете, этот идеальный распорядок дня настраивает мои внутренние часы на поддержание оптимального здоровья. Но удается ли мне соблюдать его каждый день? Конечно, нет. Моя работа связана с многочисленными разъездами не только по США, но и по всему миру. Порой я вынужден вставать очень рано, чтобы успеть на самолет или провести телеконференцию с коллегами, которые живут в других часовых поясах. Если поджимают сроки, я могу допоздна засиживаться на работе перед монитором компьютера. А иногда мне приходится нарушить режим ОВП, чтобы принять участие в развлечениях коллег или в конференции с последующим банкетом, который, как правило, проводится намного позже, чем мне хотелось бы.
И все же я каждый день изо всех сил стараюсь сделать так, чтобы как можно больше требований моего циркадного кода было выполнено с максимально возможной точностью. Если у меня нет возможности заниматься физическими упражнениями, я слежу за тем, чтобы не нарушать предписанный режимом ОВП период воздержания от пищи. Если ужинать мне приходится поздно, я все равно пытаюсь предоставить своему желудку минимум 12–13 часов отдыха перед следующим приемом пищи. Если я вынужден поздно ложиться спать, то на следующее утро обязательно занимаюсь физическими упражнениями. В общем, вы меня поняли. Мы стремимся к совершенству, но иногда приходится довольствоваться чем-то просто хорошим. Я знаю, что мое здоровье – в моих руках: если я хочу принести себе как можно больше пользы, мне нужно как можно чаще выбирать то, что правильно.
Надеюсь, что эта книга помогла вам узнать кое-что о вашем циркадном коде и о том, как легко произвести небольшие изменения, необходимые для его нормализации. После того как вы попробуете несколько недель следовать предложенным в ней рекомендациям, вернитесь к тестам, приведенным в главе 3, и посмотрите, изменились ли ваши результаты. Сохраните изначально собранные данные, чтобы вам было легче оценивать свои успехи в формировании новых привычек. Помните, что от времени, когда вы каждый день съедаете первый и последний кусочек пищи, зависит бесперебойная работа всех циркадных часов. Снижение интенсивности освещения в темное время суток, особенно уменьшение воздействия яркого света, поможет вам быстрее засыпать и дольше спать. Физические упражнения вызывают усталость и в то же время улучшают здоровье мозга – мы знаем, что основная часть работы, укрепляющей здоровье мозга, осуществляется, когда вы спите.
Доказанные полезные результаты ограничения времени питания
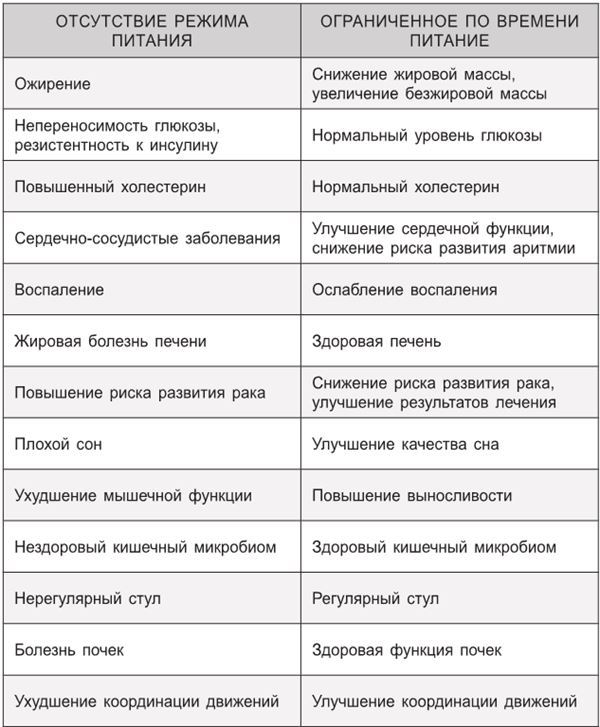
Если сейчас вы страдаете каким-нибудь хроническим заболеванием, помните, что нормализация циркадного кода является одним из самых лучших способов, позволяющих повернуть вспять его ход или ослабить степень его тяжести. Мы начинаем получать все больше благодарностей от людей, которым эти рекомендации помогли начать вести здоровый образ жизни. Некоторые даже сообщают, что им больше не нужно принимать лекарства. Роль, которую ОВП играет в синхронизации циркадного кода и улучшении здоровья, невозможно переоценить. В таблице, приведенной на странице 339, перечислены самые сильные стимулы, призванные побудить вас и ваших близких воспользоваться преимуществами ОВП.
Надеюсь, что вы не верите в существование волшебных пилюль и понимаете, что восстановление циркадного кода не станет чудодейственным лекарством от всех болезней. Но если вы объедините рекомендации своего врача с информацией, представленной в данной книге, то сделаете все от вас зависящее, чтобы улучшить состояние своего здоровья и оставаться здоровыми до конца своих дней. Разумеется, я надеюсь, что именно так вы и поступите.
Литература
Предисловие
1. F. Damiola et al., «Restricted Feeding Uncouples Circadian Oscillators in Peripheral Tissues from the Central Pacemaker in the Suprachiasmatic Nucleus», Genes and Development 14 (2000): 2950—61.
2. K. A. Stokkan et al., «Entrainment of the Circadian Clock in the Liver by Feeding», Science 291 (2001): 490—93.
3. M. P. St-Onge, et al., «Meal Timing and Frequency: Implications for Cardiovascular Disease Prevention: A Scientific Statement from the American Heart Association», Circulation 135, no. 9 (2017): e96—e121.
ГЛАВА 1. Все мы – работники со сменным графиком
1. D. Fischer et al., «Chronotypes in the US – Influence of Age and Sex», PLoS ONE 12 (2017): e0178782.
2. T. Roenneberg et al., «Epidemiology of the Human Circadian Clock», Sleep Medicine Reviews 11, no. 6 (2007): 429—38.
3. L. Kaufman, «Your Schedule Could Be Killing You», Popular Science, September/October 2017, https://www.popsci.com/your-schedule-could-be-killing-you.
4. J. Li et al., «Parents’ Nonstandard Work Schedules and Child Well-Being: A Critical Review of the Literature», Journal of Primary Prevention 35, no. 1 (2014): 53–73.
5. D. L. Brown et al., «Rotating Night Shift Work and the Risk of Ischemic Stroke», American Journal of Epidemiology 169, no. 11 (2009): 1370—77.
6. M. Conlon, N. Lightfoot, and N. Kreiger, «Rotating Shift Work and Risk of Prostate Cancer», Epidemiology 18, no. 1 (2007): 182—83.
7. S. Davis, D. K. Mirick, and R. G. Stevens, «Night Shift Work, Light at Night, and Risk of Breast Cancer», Journal of the National Cancer Institute 93, no. 20 (2001): 1557—62. 8. C. Hublin et al., «Shift-Work and Cardiovascular Disease: A Population-Based 22-Year Follow-Up Study», European Journal of Epidemiology 25, no. 5 (2010): 315—23. 9. B. Karlsson, A. Knutsson, and B. Lindahl, «Is There an Association between Shift Work and Having a Metabolic Syndrome? Results from a Population Based Study of 27,485 people», Occupational & Environmental Medicine 58, no. 11 (2001): 747—52.
10. T. A. Lahti et al., «Night-Time Work Predisposes to Non-Hodgkin Lymphoma», International Journal of Cancer 123, no. 9 (2008): 2148—51.
11. S. P. Megdal et al., «Night Work and Breast Cancer Risk: A Systematic Review and Meta-Analysis», European Journal of Cancer 41, no. 13 (2005): 2023—32.
12. F. A. Scheer et al., «Adverse Metabolic and Cardiovascular Consequences of Circadian Misalignment», Proceedings of the National Academy of Sciences of the United States of America 106, no. 11 (2009): 4453—58.
13. E. S. Schernhammer et al., «Night-Shift Work and Risk of Colorectal Cancer in the Nurses’ Health Study», Journal of the National Cancer Institute 95, no. 11 (2003): 825—28.
14. E. S. Schernhammer et al., «Rotating Night Shifts and Risk of Breast Cancer in Women Participating in the Nurses’ Health Study», Journal of the National Cancer Institute 93, no. 20 (2001): 1563—68.
15. S. Sookoian et al., «Effects of Rotating Shift Work on Biomarkers of Metabolic Syndrome and Inflammation», Journal of Internal Medicine 261, no. 3 (2007): 285—92.
16. A. N. Viswanathan, S. E. Hankinson, and E. S. Schernhammer, «Night Shift Work and the Risk of Endometrial Cancer», Cancer Research 67 no. 21 (2007): 10618—22.
17. E. S. Soteriades et al., «Obesity and Cardiovascular Disease Risk Factors in Firefighters: A Prospective Cohort Study», Obesity Research 13, no. 10 (2005): 1756—63.
18. E. S. Soteriades et al., «Cardiovascular Disease in US Firefighters: A Systematic Review», Cardiology in Review 19, no. 4 (2011): 202—15.
19. K. Straif et al., «Carcinogenicity of Shift-Work, Painting, and Fire-Fighting», Lancet Oncology 8, no. 12 (2007): 1065—66.
20. International Air Transport Association, «New Year’s Day 2014 Marks 100 Years of Commercial Aviation», press release, http:// www.iata.org/pressroom/pr/Pages/2013-12-30-01.aspx.
21. J.-J. de Mairan, «Observation Botanique», Histoire de l’Academie Royale des Sciences (1729): 35–36.
22. J. Aschoff, «Exogenous and endogenous components in circadian rhythms.» Cold Spring Harbor Symposia on Quantitative Biology 25 (1960): 11–28.
23. J. Aschoff and R. Wever, «Spontanperiodik des Menschen bei Ausschluß aller Zeitgeber», Naturwissenschaften 49, no. 15 (1962): 337—42.
24. C. J. Morris, D. Aeschbach, and F. A. Scheer, «Circadian System, Sleep, and Endocrinology», Molecular and Cellular Endocrinology 349, no. 1 (2012): 91—104.
25. R. N. Carmody and R. W. Wrangham, «The Energetic Significance of Cooking», Journal of Human Evolution 57, no. 4 (2009): 379—91.
26. R. N. Carmody, G. S. Weintraub, and R. W. Wrangham, «Energetic Consequences of Thermal and Nonthermal Food Processing», Proceedings of the National Academy of Sciences of the United States of America 108, no. 48 (2011): 19199—203.
27. P. W. Wiessner, «Embers of Society: Firelight Talk among the Ju/’hoansi Bushmen», Proceedings of the National Academy of Sciences of the United States of America 111, no. 39 (2014): 14027—35.
28. R. Fouquet and P. J. G. Pearson, «Seven Centuries of Energy Services: The Price and Use of Light in the United Kingdom (1300–2000)», Energy Journal 27, no. 1 (2006): 139—77.
29. G. Yetish et al., «Natural Sleep and Its Seasonal Variations in Three Pre-Industrial Societies», Current Biology 25, no. 21 (2015): 2862—68.
30. H. O. de la Iglesia et al., «Ancestral Sleep», Current Biology 26, no. 7 (2016): R271—72.
31. H. O. de la Iglesia et al., «Access to Electric Light Is Associated with Shorter Sleep Duration in a Traditionally Hunter-Gatherer Community», Journal of Biological Rhythms 30, no. 4 (2015): 342—50.
32. R. G. Foster et al., «Circadian Photoreception in the Retinally Degenerate Mouse (rd/rd)», Journal of Comparative Physiology A 169, no. 1 (1991): 39–50.
33. M. S. Freeman et al., «Regulation of Mammalian Circadian Behavior by Non-Rod, Non-Cone, Ocular Photoreceptors», Science 284, no. 5413 (1999): 502—4.
34. R. J. Lucas et al., «Regulation of the Mammalian Pineal by Non-Rod, Non-Cone, Ocular Photoreceptors», Science 284, no. 5413 (1999): 505—7.
35. S. Panda et al., «Melanopsin (Opn4) Requirement for Normal Light-Induced Circadian Phase Shifting», Science 298, no. 5601 (2002): 2213—16.
36. N. F. Ruby et al., «Role of Melanopsin in Circadian Responses to Light», Science 298, no. 5601 (2002): 2211—13.
37. S. Hattar et al., «Melanopsin-Containing Retinal Ganglion Cells: Architecture, Projections, and Intrinsic Photosensitivity», Science 295, no. 5557 (2002): 1065—70.
38. D. M. Berson, F. A. Dunn, and M. Takao, «Phototransduction by Retinal Ganglion Cells That Set the Circadian Clock», Science 295, no. 5557 (2002): 1070—73.
39. I. Provencio et al., «Melanopsin: An Opsin in Melanophores, Brain, and Eye», Proceedings of the National Academy of Sciences of the United States of America 95, no. 1 (1998): 340 – 45.
ГЛАВА 2. Как работают циркадные ритмы: выбор времени – это всё
1. R. J. Konopka and S. Benzer, «Clock Mutants of Drosophila melanogaster», Proceedings of the National Academy of Sciences of the United States of America 68, no. 9 (1971): 2112—16.
2. S. Panda et al., «Coordinated Transcription of Key Pathways in the Mouse by the Circadian Clock», Cell 109, no. 3 (2002): 307—20.
3. D. K. Welsh, J. S. Takahashi, and S. A. Kay, «Suprachiasmatic Nucleus: Cell Autonomy and Network Properties», Annual Review of Physiology 72 (2010): 551—77.
4. R. E. Fargason et al., «Correcting Delayed Circadian Phase with Bright Light Therapy Predicts Improvement in ADHD Symptoms: A Pilot Study», Journal of Psychiatric Research 91 (2017): 105—10.
5. T. Roenneberg et al., «Epidemiology of the Human Circadian Clock», Sleep Medicine Reviews 11, no. 6 (2007): 429—38.
6. K. L. Toh et al., «An hPer2 Phosphorylation Site Mutation in Familial Advanced Sleep Phase Syndrome», Science 291, no. 5506 (2001): 1040—43.
7. Y. He et al., «The Transcriptional Repressor DEC2 Regulates Sleep Length in Mammals», Science 325, no. 5942 (2009): 866—70.
8. K. P. Wright, Jr. et al., «Entrainment of the Human Circadian Clock to the Natural Light-Dark Cycle», Current Biology 23, no. 16 (2013): 1554—58.
9. C. Vollmers et al., «Time of Feeding and the Intrinsic Circadian Clock Drive Rhythms in Hepatic Gene Expression», Proceedings of the National Academy of Sciences of the United States of America 106, no. 50 (2009): 21453—58.
10. D. M. Edgar et al., «Influence of Running Wheel Activity on Free-Running Sleep/Wake and Drinking Circadian Rhythms in Mice», Physiology & Behavior 50, no. 2 (1991): 373—78. 11. S. Brand et al., «High Exercise Levels Are Related to Favorable Sleep Patterns and Psychological Functioning in Adolescents: A Comparison of Athletes and Controls», Journal of Adolescent Health 46, no. 2 (2010): 133 – 41.
12. K. J. Reid et al., «Aerobic Exercise Improves Self-Reported Sleep and Quality of Life in Older Adults with Insomnia», Sleep Medicine 11, no. 9 (2010): 934 – 40.
13. S. S. Tworoger et al., «Effects of a Yearlong Moderate-Intensity Exercise and a Stretching Intervention on Sleep Quality in Postmenopausal Women», Sleep 26, no. 7 (2003): 830—36.
14. E. J. van Someren et al., «Long-Term Fitness Training Improves the Circadian Rest-Activity Rhythm in Healthy Elderly Males», Journal of Biological Rhythms 12, no. 2 (1997): 146—56.
ГЛАВА 3. Проверьте и оцените: насколько оптимален ваш циркадный код?
1. F. C. Bell and M. L. Miller, «Life Tables for the United States Social Security Area 1900–2100», Social Security Administration, https://www.ssa.gov/oact/NOTES/as120/LifeTables_Body.html.
2. C. R. Marinac et al., «Prolonged Nightly Fasting and Breast Cancer Prognosis», JAMA Oncology 2, no. 8 (2016): 1049—55.
3. A. J. Davidson et al., «Chronic Jet-Lag Increases Mortality in Aged Mice», Current Biology 16, no. 21 (2006): R914—16.
4. D. C. Mohren et al., «Prevalence of Common Infections Among Employees in Difef rent Work Schedules», Journal of Occupational and Environmental Medicine 44, no. 11 (2002): 1003—11.
5. N. J. Schork, «Personalized Medicine: Time for One-Person Trials», Nature 520, no. 7549 (2015): 609—11.
6. B. J. Hahm et al., «Bedtime Misalignment and Progression of Breast Cancer», Chronobiology International 31, no. 2 (2014): 214—21.
7. E. L. McGlinchey et al., «The Effect of Sleep Deprivation on Vocal Expression of Emotion in Adolescents and Adults», Sleep 34, no. 9 (2011): 1233— 41.
8. S. J. Wilson et al., «Shortened Sleep Fuels Inflammatory Responses to Marital Conflict: Emotion Regulation Matters», Psychoneuroendocrinology 79 (2017): 74–83. 9. S. Gill and S. Panda, «A Smartphone App Reveals Erratic Diurnal Eating Patterns in Humans That Can Be Modulated for Health Benefits», Cell Metabolism 22, no. 5 (2015): 789—98.
10. Ibid.
11. N. J. Gupta, V. Kumar, and S. Panda, «A Camera-Phone Based Study Reveals Erratic Eating Pattern and Disrupted Daily Eating-Fasting Cycle among Adults in India», PLoS ONE 12, no. 3 (2017): e0172852.
12. M. Ohayon et al., «National Sleep Foundation’s Sleep Quality Recommendations: First Report», Sleep Health 3, no. 1 (2017): 6—19.
13. M. Hirshkowitz et al., «National Sleep Foundation’s Sleep Time Duration Recommendations: Methodology and Results Summary», Sleep Health 1, no. 1 (2015): 40–43.
14. M. Hirshkowitz et al., «National Sleep Foundation’s Updated Sleep Duration Recommendations: Final Report», Sleep Health 1, no. 4 (2015): 233—43.
ГЛАВА 4. Циркадный код для улучшения ночного сна
1. M. Hirshkowitz et al., «National Sleep Foundation’s Sleep Time Duration Recommendations: Methodology and Results Summary», Sleep Health 1, no. 1 (2015): 40–43.
2. M. Hirshkowitz et al., «National Sleep Foundation’s Updated Sleep Duration Recommendations: Final Report», Sleep Health 1, no. 4 (2015): 233— 43.
3. D. F. Kripke et al., «Mortality Associated with Sleep Duration and Insomnia», Archives of General Psychiatry 59, no. 2 (2002): 131—36.
4. G. Yetish et al., «Natural Sleep and Its Seasonal Variations in Three Pre-Industrial Societies», Current Biology 25, no. 21 (2015): 2862—68.
5. H. O. de la Iglesia et al., «Access to Electric Light Is Associated with Shorter Sleep Duration in a Traditionally Hunter-Gatherer Community», Journal of Biological Rhythms 30, no. 4 (2015): 342—50. 6. A. M. Williamson and A. M. Feyer, «Moderate Sleep Deprivation Produces Impairments in Cognitive and Motor Performance Equivalent to Legally Prescribed Levels of Alcohol Intoxication», Occupational & Environmental Medicine 57, no. 10 (2000): 649—55. 7. H. P. van Dongen et al., «The Cumulative Cost of Additional Wakefulness: Dose-Response Effects on Neurobehavioral Functions and Sleep Physiology from Chronic Sleep Restriction and Total Sleep Deprivation», Sleep 26, no. 2 (2003): 117—26. 8. R. E. Fargason et al., «Correcting Delayed Circadian Phase with Bright Light Therapy Predicts Improvement in ADHD Symptoms: A Pilot Study», Journal of Psychiatric Research 91 (2017): 105—10. 9. N. Kronfeld-Schor and H. Einat, «Circadian Rhythms and Depression: Human Psychopathology and Animal Models», Neuropharmacology 62, no. 1 (2012): 101—14.
10. M. E. Coles, J. R. Schubert, and J. A. Nota, «Sleep, Circadian Rhythms, and Anxious Traits», Current Psychiatry Reports 17, no. 9 (2015): 73.
11. S. E. Anderson et al., «Self-Regulation and Household Routines at Age Three and Obesity at Age Eleven: Longitudinal Analysis of the UK Millennium Cohort Study», International Journal of Obesity 41, no. 10 (2017): 1459—66.
12. A. W. McHill et al., «Impact of Circadian Misalignment on Energy Metabolism during Simulated Nightshift Work», Proceedings of the National Academy of Sciences of the United States of America 111, no. 48 (2014): 17302—7.
13. B. Martin, M. P. Mattson, and S. Maudsley, «Caloric Restriction and Intermittent Fasting: Two Potential Diets for Successful Brain Aging», Ageing Research Reviews 5, no. 3 (2006): 332—53.
14. S. Gill and S. Panda, «A Smartphone App Reveals Erratic Diurnal Eating Patterns in Humans That Can Be Modulated for Health Benefits», Cell Metabolism 22, no. 5 (2015): 789—98.
15. S. J. Crowley and C. I. Eastman, «Human Adolescent Phase Response Curves to Bright White Light», Journal of Biological Rhythms 32, no. 4 (2017): 334— 44.
16. J. A. Evans et al., «Dim Nighttime Illumination Alters Photoperiodic Responses of Hamsters through the Intergeniculate Leaflet and Other Photic Pathways», Neuroscience 202 (2012): 300–308.
17. L. S. Gaspar et al., «Obstructive Sleep Apnea and Hallmarks of Aging», Trends in Molecular Medicine 23, no. 8 (2017): 675—92.
18. E. Ferracioli-Oda, A. Qawasmi, and M. H. Bloch, «Meta-Analysis: Melatonin for the Treatment of Primary Sleep Disorders», PLoS ONE 8, no. 5 (2013): e63773.
ГЛАВА 5. Ограничение времени питания: настройте свои часы на снижение веса
1. C. M. McCay and M. F. Crowell, «Prolonging the Life Span», Scientific Monthly 39, no. 5 (1934): 405—14.
2. S. K. Das, P. Balasubramanian, and Y. K. Weerasekara, «Nutrition Modulation of Human Aging: The Calorie Restriction Paradigm», Molecular and Cellular Endocrinology 455 (2017): 148—57.
3. A. Kohsaka et al., «High-Fat Diet Disrupts Behavioral and Molecular Circadian Rhythms in Mice», Cell Metabolism 6, no. 5 (2007): 414—21.
4. M. Hatori et al., «Time-Restricted Feeding without Reducing Caloric Intake Prevents Metabolic Diseases in Mice Fed a High-Fat Diet», Cell Metabolism 15, no. 6 (2012): 848—60.
5. A. Chaix et al., «Time-Restricted Feeding Is a Preventative and Therapeutic Intervention against Diverse Nutritional Challenges», Cell Metabolism 20, no. 6 (2014): 991—1005.
6. A. Zarrinpar et al., «Diet and Feeding Pattern Affect the Diurnal Dynamics of the Gut Microbiome», Cell Metabolism 20, no. 6 (2014): 1006—17.
7. V. A. Acosta-Rodriguez et al., «Mice under Caloric Restriction Self-Impose a Temporal Restriction of Food Intake as Revealed by an Automated Feeder System», Cell Metabolism 26, no. 1 (2017): 267—77.e2. 8. M. Garaulet et al., «Timing of Food Intake Predicts Weight Loss Effectiveness», International Journal of Obesity 37, no. 4 (2013): 604—11. 9. S. Gill and S. Panda, «A Smartphone App Reveals Erratic Diurnal Eating Patterns in Humans That Can Be Modulated for Health Benefits», Cell Metabolism 22, no. 5 (2015): 789—98.
10. T. Moro et al., «Effects of Eight Weeks of Time-Restricted Feeding (16/8) on Basal Metabolism, Maximal Strength, Body Composition, Inflammation, and Cardiovascular Risk Factors in Resistance-Trained Males», Journal of Translational Medicine 14 (2016): 290.
11. J. Rothschild et al., «Time-Restricted Feeding and Risk of Metabolic Disease: A Review of Human and Animal Studies», Nutrition Reviews 72, no. 5 (2014): 308—18.
12. T. Ruiz-Lozano et al., «Timing of Food Intake Is Associated with Weight Loss Evolution in Severe Obese Patients after Bariatric Surgery», Clinical Nutrition 35, no. 6 (2016): 1308—14.
13. A. W. McHill et al., «Later Circadian Timing of Food Intake Is Associated with Increased Body Fat», American Journal of Clinical Nutrition 106, no. 6 (2017): 1213—19.
14. National Institute of Diabetes and Digestive and Kidney Diseases, «Digestive Diseases Statistics for the United States», https:// www.niddk.nih.gov/health-information/health-statistics/digestive-diseases.
15. McHill, «Later Circadian Timing.»
16. J. Suez et al., «Artificial Sweeteners Induce Glucose Intolerance by Altering the Gut Microbiota», Nature 514, no. 7521 (2014): 181—86.
ГЛАВА 6. Оптимизация обучения и работы
1. J. S. Durmer and D. F. Dinges, «Neurocognitive Consequences of Sleep Deprivation», Seminars in Neurology 25, no. 1 (2005): 117—29. 2. S. M. Greer, A. N. Goldstein, and M. P. Walker, «The Impact of Sleep Deprivation on Food Desire in the Human Brain», Nature Communications 4 (2013): article no. 2259. 3. R. Stickgold, «Sleep-Dependent Memory Consolidation», Nature 437, no. 7063 (2005): 1272—78. 4. T. A. LeGates et al., «Aberrant Light Directly Impairs Mood and Learning through Melanopsin-Expressing Neurons», Nature 491, no. 7425 (2012): 594—98. 5. M. Boubekri, et al., «Impact of Windows and Daylight Exposure on Overall Health and Sleep Quality of Ofifce Workers: A Case-Control Pilot Study», Journal of Clinical Sleep Medicine 10, no. 6 (2014): 603—11. 6. P. Meerlo, A. Sgoifo, and D. Suchecki, «Restricted and Disrupted Sleep: Effects on Autonomic Function, Neuroendocrine Stress Systems and Stress Responsivity», Sleep Medicine Reviews 12, no. 3 (2008): 197–210. 7. J. A. Foster and K. A. McVey Neufeld, «Gut-Brain Axis: How the Microbiome Influences Anxiety and Depression», Trends in Neurosciences 36, no. 5 (2013): 305—12. 8. S. J. Kentish and A. J. Page, «Plasticity of Gastro-Intestinal Vagal Afferent Endings», Physiology & Behavior 136 (2014): 170—78. 9. L. A. Reyner et al., «‘Post-Lunch’ Sleepiness During Prolonged, Monotonous Driving – Effects of Meal Size», Physiology & Behavior 105, no. 4 (2012): 1088—91.
10. M. S. Ganio, et al., «Mild Dehydration Impairs Cognitive Performance and Mood of Men», British Journal of Nutrition 106, no. 10 (2011): 1535— 43.
11. T. Partonen and J. Lönnqvist, «Bright Light Improves Vitality and Alleviates Distress in Healthy People», Journal of Affective Disorders 57, no. 1–3 (2000): 55–61.
12. D. H. Avery et al., «Bright Light Therapy of Subsyndromal Seasonal Affective Disorder in the Workplace: Morning vs. Afternoon Exposure», Acta Psychiatrica Scandinavica 103, no. 4 (2001): 267—74.
13. C. Cajochen et al., «Evening Exposure to a Light-Emitting Diodes (LED)-Backlit Computer Screen Affects Circadian Physiology and Cognitive Performance», Journal of Applied Physioliology 110, no. 5 (2011): 1432—38.
14. A. M. Chang et al., «Evening Use of Light-Emitting eReaders Negatively Affects Sleep, Circadian Timing, and Next-Morning Alertness», Proceedings of the National Academy of Sciences of the United States of America 112, no. 4 (2015): 1232—37.
15. M. P. Mattson and R. Wan, «Beneficial Effects of Intermittent Fasting and Caloric Restriction on the Cardiovascular and Cerebrovascular Systems», Journal of Nutritional Biochemistry 16, no. 3 (2005): 129—37.
16. R. K. Dishman et al., «Neurobiology of Exercise», Obesity 14, no. 3 (2006): 345—56.
17. E. Guallar, «Coffee Gets a Clean Bill of Health», BMJ 359 (2017):j5356.
18. R. Poole et al., «Coffee Consumption and Health: Umbrella Review of Meta-Analyses of Multiple Health Outcomes», BMJ 359 (2017):j5024.
19. I. Clark and H. P. Landolt, «Coffee, Caffeine, and Sleep: A Systematic Review of Epidemiological Studies and Randomized Controlled Trials», Sleep Medicine Reviews 31 (2017): 70–78.
20. J. Shearer and T. E. Graham, «Performance Effects and Metabolic Consequences of Caffeine and Caffeinated Energy Drink Consumption on Glucose Disposal», Nutrition Reviews 72, Suppl. 1 (2014): 121—36.
21. T. M. Burke et al., «Effects of Caffeine on the Human Circadian Clock In Vivo and In Vitro», Science Translational Medicine 7, no. 35 (2015): 305ra146.
22. S. Grossman, «These Are the Most Popular Starbucks Drinks Across the U.S.», Time, July 1, 2014.
23. H. P. van Dongen and D. F. Dinges, «Sleep, Circadian Rhythms, and Psychomotor Vigilance», Clinics in Sports Medicine 24, no. 2 (2005): 237— 49.
24. B. L. Smarr, «Digital Sleep Logs Reveal Potential Impacts of Modern Temporal Structure on Class Performance in Different Chronotypes», Journal of Biological Rhythms 30, no. 1 (2015): 61–67.
25. K. Wahlstrom, «Changing Times: Findings from the First Longitudinal Study of Later High School Start Times», National Association of Secondary School Principals Bulletin 86, no. 633 (2002): 3—21.
26. J. Boergers, C. J. Gable, and J. A. Owens, «Later School Start Time Is Associated with Improved Sleep and Daytime Functioning in Adolescents», Journal of Developmental and Behavioral Pediatrics 35, no. 1 (2014): 11–17.
27. J. A. Owens, K. Belon, and P. Moss, «Impact of Delaying School Start Time on Adolescent Sleep, Mood, and Behavior», Archives of Pediatric & Adolescent Medicine 164, no. 7 (2010): 608—14.
ГЛАВА 7. Как синхронизировать физические упражнения со своим циркадным кодом
1. M. S. Tremblay et al., «Physiological and Health Implications of a Sedentary Lifestyle», Applied Physiology, Nutrition, and Metabolism 35, no. 6 (2010): 725— 40.
2. T. Althoff et al., «Large-Scale Physical Activity Data Reveal Worldwide Activity Inequality», Nature 547, no. 7663 (2017): 336—39.
3. D. R. Bassett, P. L. Schneider, and G. E. Huntington, «Physical Activity in an Old Order Amish Community», Medicine and Science in Sports and Exercise 36, no. 1 (2004): 79–85.
4. H. O. de la Iglesia et al., «Access to Electric Light Is Associated with Shorter Sleep Duration in a Traditionally Hunter-Gatherer Community», Journal of Biological Rhythms 30, no. 4 (2015): 342—50.
5. T. Kubota et al., «Interleukin-15 and Interleukin-2 Enhance Non-REM Sleep in Rabbits», American Journal of Physiology: Regulatory Integrative and Comparative Physiology 281, no. 3 (2001): R1004—12. 6. Y. Li et al., «Association of Serum Irisin Concentrations with the Presence and Severity of Obstructive Sleep Apnea Syndrome», Journal of Clinical Laboratory Analysis 31, no. 5 (2016): e22077. 7. K. M. Awad et al., «Exercise Is Associated with a Reduced Incidence of Sleep-Disordered Breathing», American Journal of Medicine 125, no. 5 (2012): 485—90. 8. J. C. Ehlen et al., «Bmal1 Function in Skeletal Muscle Regulates Sleep», eLife 6 (2017): e26557. 9. E. Steidle-Kloc et al., «Does Exercise Training Impact Clock Genes in Patients with Coronary Artery Disease and Type 2 Diabetes Mellitus?» European Journal of Preventive Cardiology 23, no. 13 (2016): 1375—82.
10. N. Yang, and Q. J. Meng, «Circadian Clocks in Articular Cartilage and Bone: A Compass in the Sea of Matrices», Journal of Biological Rhythms 31, no. 5 (2016): 415—27.
11. E. A. Schroder et al., «Intrinsic Muscle Clock Is Necessary for Musculoskeletal Health», Journal of Physiology 593, no. 24 (2015): 5387—404.
12. S. Aoyama and S. Shibata, «The Role of Circadian Rhythms in Muscular and Osseous Physiology and Their Regulation by Nutrition and Exercise», Frontiers in Neuroscience 11 (2017): article no. 63.
13. E. Woldt et al., «Rev-erb-α Modulates Skeletal Muscle Oxidative Capacity by Regulating Mitochondrial Biogenesis and Autophagy», Nature Medicine 19, no. 8 (2013): 1039—46.
14. H. van Praag et al., «Running Enhances Neurogenesis, Learning, and Long-Term Potentiation in Mice», Proceedings of the National Academy of Sciences of the United States of America 96, no. 23 (1999): 13427—31.
15. J. L. Yang et al., «BDNF and Exercise Enhance Neuronal DNA Repair by Stimulating CREB-Mediated Production of Apurinic/
Apyrimidinic Endonuclease 1», NeuroMolecular Medicine 16, no. 1 (2014): 161—74.
16. S. M. Nigam et al., «Exercise and BDNF Reduce Αβ Production by Enhancing Α-Secretase Processing of APP», Journal of Neurochemistry 142, no. 2 (2017): 286—96.
17. W. D. van Marken Lichtenbelt et al., «Cold-Activated Brown Adipose Tissue in Healthy Men», New England Journal of Medicine 360, no. 15 (2009): 1500–1508.
18. V. Ouellet et al., «Brown Adipose Tissue Oxidative Metabolism Contributes to Energy Expenditure During Acute Cold Exposure in Humans», Journal of Clinical Investigation 122, no. 2 (2012): 545—52.
19. E. Thun et al., «Sleep, Circadian Rhythms, and Athletic Performance», Sleep Medicine Reviews 23 (2015): 1–9.
20. E. Facer-Childs and R. Brandstaetter, «The Impact of Circadian Phenotype and Time Since Awakening on Diurnal Performance in Athletes», Current Biology 25, no. 4 (2015): 518—22.
21. R. S. Smith, C. Guilleminault, and B. Efron, «Circadian Rhythms and Enhanced Athletic Performance in the National Football League», Sleep 20, no. 5 (1997): 362— 65.
22. N. A. King, V. J. Burley, and J. E. Blundell, «Exercise-Induced Suppression of Appetite: Effects on Food Intake and Implications for Energy Balance», European Journal of Clinical Nutrition 48, no. 10 (1994): 715—24.
23. E. A. Richter and M. Hargreaves, «Exercise, GLUT4, and Skeletal Muscle Glucose Uptake», Physiological Reviews 93, no. 3 (2013): 993—1017.
24. E. van Cauter et al., «Nocturnal Decrease in Glucose Tolerance during Constant Glucose Infusion», Journal of Clinical Endocrinology and Metabolism 69, no. 3 (189): 604—11.
25. J. Sturis et al., «24-Hour Glucose Profiles during Continuous or Oscillatory Insulin Infusion: Demonstration of the Functional Significance of Ultradian Insulin Oscillations», Journal of Clinical Investigation 95, no. 4 (1995): 1464—71.
26. H. H. Fullagar et al., «Sleep and Athletic Performance: The Effects of Sleep Loss on Exercise Performance, and Physiological and Cognitive Responses to Exercise», Sports Medicine 45, no. 2 (2015): 161—86.
27. A. Chaix et al., «Time-Restricted Feeding Is a Preventative and Therapeutic Intervention against Diverse Nutritional Challenges», Cell Metabolism 20, no. 6 (2014): 991—1005.
28. T. Moro et al., «Effects of Eight Weeks of Time-Restricted Feeding (16/8) on Basal Metabolism, Maximal Strength, Body Composition, Inflammation, and Cardiovascular Risk Factors in Resistance-Trained Males», Journal of Translational Medicine 14 (2016): article no. 290.
29. P. Puchalska and P. A. Crawford, «Multi-Dimensional Roles of Ketone Bodies in Fuel Metabolism, Signaling, and Therapeutics», Cell Metabolism 25, no. 2 (2017): 262—84.
30. King, Burley, and Blundell, «Exercise-Induced Suppression.»
ГЛАВА 8. Возьмите под контроль главных нарушителей: источники освещения и дисплеи
1. R. M. Lunn et al., «Health Consequences of Electric Lighting Practices in the Modern World: A Report on the National Toxicology Program’s Workshop on Shift Work at Night, Artificial Light at Night, and Circadian Disruption», Science of Total Environment 607—8 (2017): 1073—84.
2. C. A. Czeisler et al., «Bright Light Induction of Strong (Type 0) Resetting of the Human Circadian Pacemaker», Science 244, no. 4910 (1989): 1328—33.
3. J. Xu et al., «Altered Activity-Rest Patterns in Mice with a Human Autosomal-Dominant Nocturnal Frontal Lobe Epilepsy Mutation in the β2 Nicotinic Receptor», Molecular Psychiatry 16, no. 10 (2011): 1048—61.
4. L. A. Kirkby and M. B. Feller, «Intrinsically Photosensitive Ganglion Cells Contribute to Plasticity in Retinal Wave Circuits», Proceedings of the National Academy of Sciences of the United States of America 110, no. 29 (2013): 12090—95.
5. J. M. Renna, S. Weng, and D. M. Berson, «Light Acts through Melanopsin to Alter Retinal Waves and Segregation of Retinogeniculate Afferents», Nature Neuroscience 14, no. 7 (2011): 827—29. 6. J. Parent, W. Sanders, and R. Forehand, «Youth Screen Time and Behavioral Health Problems: The Role of Sleep Duration and Disturbances», Journal of Developmental and Behavioral Pediatrics 37, no. 4 (2016): 277—84. 7. The Nielsen Total Audience Report: Q2 2017, http://www. nielsen.com/us/en/insights/reports/2017/the-nielsen-total-audience-q2-2017.html. 8. I. Provencio et al., «Melanopsin: An Opsin in Melanophores, Brain, and Eye», Proceedings of the National Academy of Sciences of the United States of America 95, no. 1 (1998): 340— 45. 9. P. A. Good, R. H. Taylor, and M. J. Mortimer, «The use of tinted glasses in childhood migraine.» Headache 31 (1991): 533—36.
10. S. Vásquez-Ruiz et al., «A Light/Dark Cycle in the NICU Accelerates Body Weight Gain and Shortens Time to Discharge in Preterm Infants», Early Human Development 90, no. 9 (2014): 535— 40.
11. P. A. Regidor et al., «Identification and Prediction of the Fertile Window with a New Web-Based Medical Device Using a Vaginal Biosensor for Measuring the Circadian and Circamensual Core Body Temperature», Gynecological Endocrinology 34, no. 3 (2018): 256—60.
12. X. Li et al., «Digital Health: Tracking Physiomes and Activity Using Wearable Biosensors Reveals Useful Health-Related Information», PLoS Biology 15, no. 1 (2017): e2001402.
13. C. Skarke et al., «A Pilot Characterization of the Human Chronobiome», Scientific Reports 7 (2017): article no. 17141.
14. D. Zeevi et al., «Personalized Nutrition by Prediction of Glycemic Responses», Cell 163, no. 5 (2015): 1079—94.
ГЛАВА 9. Внутренние часы, микробиом и проблемы с пищеварением
1. J. G. Moore, «Circadian Dynamics of Gastric Acid Secretion and Pharmacodynamics of H2 Receptor Blockade», Annals of the New York Academy of Sciences 618 (1991): 150—58.
2. K. Spiegel et al., «Brief Communication: Sleep Curtailment in Healthy Young Men Is Associated with Decreased Leptin Levels, Elevated Ghrelin Levels, and Increased Hunger and Appetite», Annals of Internal Medicine 141, no. 11 (2004): 846—50.
3. S. Taheri et al., «Short Sleep Duration Is Associated with Reduced Leptin, Elevated Ghrelin, and Increased Body Mass Index», PLoS Medicine 1, no. 3 (2004): e62.
4. J. Bradwejn, D. Koszycki, and G. Meterissian, Cholecystokinin-tetrapeptide Induces Panic Attacks in Patients with Panic Disorder. Can J Psychiatry 35 (1990): 83–85.
5. L. M. Ubaldo-Reyes, R. M. Buijs, C. Escobar, and M. Angeles-Castellanos, «Scheduled Meal Accelerates Entrainment to a 6-H
Phase Advance by Shifting Central and Peripheral Oscillations in Rats», European Journal of Neuroscience 46, no. 3 (2017): 1875—86.
6. C. A. Thaiss et al., «Transkingdom Control of Microbiota Diurnal Oscillations Promotes Metabolic Homeostasis», Cell 159, no. 3 (2014): 514—29.
7. P. J. Turnbaugh et al., «Diet-Induced Obesity is Linked to Marked but Reversible Alterations in the Mouse Distal Gut Microbiome», Cell Host & Microbe 3, no. 4 (2008): 213—23.
8. Thaiss, «Transkingdom Control of Microbiota Diurnal Oscillations.»
9. A. Zarrinpar et al., «Diet and Feeding Pattern Affect the Diurnal Dynamics of the Gut Microbiome», Cell Metabolism 20, no. 6
(2014): 1006—17. 10. J. A. Foster and K. A. McVey Neufeld, «Gut-Brain Axis: How the Microbiome Influences Anxiety and Depression», Trends in
Neurosciences 36, no. 5 (2013): 305—12.
11. D. Hranilovic et al., «Hyperserotonemia in Adults with Autistic Disorder», Journal of Autism and Developmental Disorders 37, no. 10 (2007): 1934— 40.
12. D. F. MacFabe et al., «Effects of the Enteric Bacterial Metabolic Product Propionic Acid on Object-Directed Behavior, Social Behavior, Cognition, and Neuroinflammation in Adolescent Rats: Relevance to Autism Spectrum Disorder», Behavioural Brain Research 217, no. 1 (2011): 47–54.
13. B. Chassaing et al., «Dietary Emulsifiers Impact the Mouse Gut Microbiota Promoting Colitis and Metabolic Syndrome», Nature 519, no. 7541 (2015): 92–96.
14. B. Chassaing et al., «Dietary Emulsifiers Directly Alter Human Microbiota Composition and Gene Expression Ex Vivo Potentiating Intestinal Inflammation», Gut 66, no. 8 (2017): 1414—27.
15. M. S. Desai et al., «A Dietary Fiber – Deprived Gut Microbiota Degrades the Colonic Mucus Barrier and Enhances Pathogen Susceptibility», Cell 167, no. 5 (2016): 1339—53.
16. K. Segawa et al., «Peptic Ulcer Is Prevalent among Shift Workers», Digestive Diseases and Sciences 32, no. 5 (1987): 449—53.
17. R. Shaker et al., «Nighttime Heartburn Is an Under-Appreciated Clinical Problem That Impacts Sleep and Daytime Function: The Results of a Gallup Survey Conducted on Behalf of the American Gastroenterological Association», American Journal of Gastroenterology 98, no. 7 (2003): 1487—93.
18. J. Leonard, J. K. Marshall, and P. Moayyedi, «Systematic Review of the Risk of Enteric Infection in Patients Taking Acid Suppression», American Journal of Gastroenterology 102, no. 9 (2007): 2047—56.
19. R. J. Hassing et al., «Proton Pump Inhibitors and Gastroenteritis», European Journal of Epidemiology 31, no. 10 (2016): 1057—63.
20. T. Antoniou et al., «Proton Pump Inhibitors and the Risk of Acute Kidney Injury in Older Patients: A Population-Based Cohort Study», CMAJ Open 3, no. 2 (2015): E166 —71.
21. M. L. Blank et al., «A Nationwide Nested Case-Control Study Indicates an Increased Risk of Acute Interstitial Nephritis with Proton Pump Inhibitor Use», Kidney International 86, no. 4 (2014): 837— 44.
22. P. Malfertheiner, A. Kandulski, and M. Venerito, «Proton-Pump Inhibitors: Understanding the Complications and Risks», Nature Reviews: Gastroenterology & Hepatology 14, no. 12 (2017): 697–710.
23. T. Ito and R. T. Jensen, «Association of Long-Term Proton Pump Inhibitor Therapy with Bone Fractures and Effects on Absorption of Calcium, Vitamin B12, Iron, and Magnesium», Current Gastroenterology Reports 12, no. 6 (2010): 448—57.
ГЛАВА 10. Роль циркадного кода в борьбе с метаболическим синдромом: ожирением, диабетом и сердечно-сосудистыми заболеваниями
1. National Institute of Diabetes and Digestive and Kidney Diseases,
«Health Risks of Being Overweight», https://www.niddk.nih.gov/ health-information/weight-management/health-risks-overweight.
2. Y. Ma et al., «Association Between Eating Patterns and Obesity in a Free-Living US Adult Population», American Journal of Epidemiology 158, no. 1 (2003): 85–92.
3. A. K. Kant and B. I. Graubard, «40-Year Trends in Meal and Snack Eating Behaviors of American Adults», Journal of the Academy of Nutrition and Dietetics 115, no. 1 (2015): 50–63.
4. S. Gill and S. Panda, «A Smartphone App Reveals Erratic Diurnal Eating Patterns in Humans That Can Be Modulated for Health Benefits», Cell Metabolism 22, no. 5 (2015): 789—98.
5. N. J. Gupta, V. Kumar, and S. Panda, «A Camera-Phone Based Study Reveals Erratic Eating Pattern and Disrupted Daily Eating-Fasting Cycle among Adults in India», PLoS ONE 12, no. 3 (2017): e0172852.
6. A. J. Stunkard, W. J. Grace, and H. G. Wolff, «The Night-Eating Syndrome: A Pattern of Food Intake among Certain Obese Patients», American Journal of Medicine 19, no. 1 (1955): 78–86.
7. E. Takeda et al., «Stress Control and Human Nutrition», Journal of Medical Investigation 51, no. 3–4 (2004): 139— 45. 8. Z. Liu et al., «PER1 Phosphorylation Specifies Feeding Rhythm in Mice», Cell Reports 7, no. 5 (2014): 1509—20. 9. T. Tuomi et al., «Increased Melatonin Signaling Is a Risk Factor for Type 2 Diabetes», Cell Metabolism 23, no. 6 (2016): 1067—77.
10. M. Watanabe et al., «Bile Acids Induce Energy Expenditure by Promoting Intracellular Thyroid Hormone Activation», Nature 439, no. 7075 (2006): 484—89.
11. A. Chaix et al., «Time-Restricted Feeding Is a Preventative and Therapeutic Intervention against Diverse Nutritional Challenges», Cell Metabolism 20, no. 6 (2014): 991—1005.
12. P. N. Hopkins, «Molecular Biology of Atherosclerosis», Physiological Reviews 93, no. 3 (2013): 1317–1542.
13. D. Montaigne et al., «Daytime Variation of Perioperative Myocardial Injury in Cardiac Surgery and Its Prevention by Rev-Erbα Antagonism: A Single-Centre Propensity-Matched Cohort Study and a Randomised Study», Lancet 391, no. 10115 (2017): 59–69.
ГЛАВА 11. Укрепление иммунной системы и лечение рака
1. C. N. Bernstein et al., «Cancer Risk in Patients with Inflammatory Bowel Disease: A Population-Based Study», Cancer 91, no. 4 (2001): 854—62. 2. N. B. Milev and A. B. Reddy, «Circadian Redox Oscillations and Metabolism», Trends in Endocrinology and Metabolism 26, no. 8 (2015): 430—37. 3. N. Martinez-Lopez et al., «System-Wide Benefits of Internal Fasting by Autophagy», Cell Metabolism 26, no. 6 (2017): 856 —71. 4. D. Cai et al., «Local and Systemic Insulin Resistance Resulting from Hepatic Activation of IKK-beta and NF-kappaB», Nature Medicine 11, no. 2 (2005): 183—90.
5. R. Narasimamurthy et al., «Circadian Clock Protein Cryptochrome Regulates the Expression of Proinflammatory Cytokines», Proceedings of the National Academy of Sciences of the United States of America 109, no. 31 (2012): 12662—67. 6. T. D. Girard et al., «Delirium as a Predictor of Long-Term Cognitive Impairment in Survivors of Critical Illness», Critical Care Medicine 38, no. 7 (2010): 1513—20. 7. S. Arumugam et al., «Delirium in the Intensive Care Unit», Journal of Emergencies, Trauma, and Shock 10, no. 1 (2017): 37–46. 8. B. van Rompaey et al., «The Effect of Earplugs during the Night on the Onset of Delirium and Sleep Perception: A Randomized Controlled Trial in Intensive Care Patients», Critical Care 16, no. 3 (2012): article no. R73. 9. A. Reinberg and F. Levi, «Clinical Chronopharmacology with Special Reference to NSAIDs», Scandinavian Journal of Rheumatology: Supplement 65 (1987): 118—22.
10. I. C. Chikanza, «Defective Hypothalamic Response to Immune and Inflammatory Stimuli in Patients with Rheumatoid Arthritis», Arthritis Rheumatism 35, no. 11 (1992): 1281—88.
11. F. Buttgereit et al., «Efifcacy of Modified-Release versus Standard Prednisone to Reduce Duration of Morning Stiffness of the Joints in Rheumatoid Arthritis (CAPRA-1): A Double-Blind, Randomised Controlled Trial», Lancet 371, no. 9608 (2008): 205—14.
12. A. Ballesta et al., «Systems Chronotherapeutics», Pharmacological Reviews 69, no. 2 (2017): 161—99.
13. K. Spiegel, J. F. Sheridan, and E. van Cauter, «Effect of Sleep Deprivation on Response to Immunization», JAMA: The Journal of the American Medical Association 288, no. 12 (2002): 1471—72.
14. J. E. Long et al., «Morning Vaccination Enhances Antibody Response over Afternoon Vaccination: A Cluster-Randomised Trial», Vaccine 34, no. 24 (2016): 2679—85.
15. O. Castanon-Cervantes, «Dysregulation of Inflammatory Responses by Chronic Circadian Disruption», Journal of Immunology 185, no. 10 (2010): 5796—805.
16. Y. M. Cissé et al., «Time-Restricted Feeding Alters the Innate Immune Response to Bacterial Endotoxin», Journal of Immunology 200, no. 2 (2018): 681—87.
17. J. Samulin Erdem et al., «Mechanisms of Breast Cancer Risk in Shift Workers: Association of Telomere Shortening with the Duration and Intensity of Night Work», Cancer Medicine 6, no. 8 (2017): 1988—97.
18. C. R. Marinac et al., «Prolonged Nightly Fasting and Breast Cancer Risk: Findings from NHANES (2009–2010)», Cancer Epidemiology, Biomarkers & Prevention 24, no. 5 (2015): 783—89.
19. E. Filipski et al., «Effects of Light and Food Schedules on Liver and Tumor Molecular Clocks in Mice», Journal of the National Cancer Institute 97, no. 7 (2005): 507—17.
20. M. W. Wu et al., «Effects of Meal Timing on Tumor Progression in Mice», Life Sciences 75, no. 10 (2004): 1181—93.
21. W. J. Hrushesky, «Circadian Timing of Cancer Chemotherapy», Science 228, no. 4695 (1985): 73–75.
22. R. Dallmann, A. Okyar, and F. Levi, «Dosing-Time Makes the Poison: Circadian Regulation and Pharmacotherapy», Trends in Molecular Medicine 22, no. 5 (2016): 430—35.
23. F. Levi et al., «Oxaliplatin Activity Against Metastatic Colorectal Cancer. A Phase II Study of 5-Day Continuous Venous Infusion at Circadian Rhythm Modulated Rate», European Journal of Cancer 29A, no. 9 (1993): 1280—84.
24. T. Matsuo et al., «Control Mechanism of the Circadian Clock for Timing of Cell Division In Vivo», Science 302, no. 5643 (2003): 255—59.
25. M. V. Plikus et al., «Local Circadian Clock Gates Cell Cycle Progression of Transient Amplifying Cells during Regenerative Hair Cycling», Proceedings of the National Academy of Sciences of the United States of America 110, no. 23 (2013): E2106—15.
26. S. Kiessling et al., «Enhancing Circadian Clock Function in Cancer Cells Inhibits Tumor Growth», BMC Biology 15 (2017): article no. 13.
27. G. Sulli et al., «Pharmacological Activation of REV-ERBs Is Lethal in Cancer and Oncogene-Induced Senescence», Nature 553, no. 7688 (2018): 351—55.
28. J. Marescaux et al., «Transatlantic Robot-Assisted Telesurgery», Nature 413, no. 6854 (2001): 379—80.
29. J. Marescaux et al., «Transcontinental Robot-Assisted Remote Telesurgery: Feasibility and Potential Applications», Annals of Surgery 235, no. 4 (2002): 487—92.
30. C. R. Marinac et al., «Prolonged Nightly Fasting and Breast Cancer Prognosis», JAMA Oncology 2, no. 8 (2016): 1049—55.
ГЛАВА 12. Роль циркадного кода в оптимизации здоровья мозга
1. P. S. Eriksson et al., «Neurogenesis in the Adult Human Hippocampus», Nature Medicine 4, no. 11 (1998): 1313—17. 2. R. Noseda et al., «A Neural Mechanism for Exacerbation of Headache by Light», Nature Neuroscience 13, no. 2 (2010): 239— 45. 3. J. Kim et al., «Implications of Circadian Rhythm in Dopamine and Mood Regulation», Molecules and Cells 40, no. 7 (2017): 450—56. 4. G. E. Davis and W. E. Lowell, «Evidence That Latitude Is Directly Related to Variation in Suicide Rates», Canadian Journal of Psychiatry 47, no. 6 (2002): 572—74. 5. T. Terao et al., «Effect of Latitude on Suicide Rates in Japan», Lancet 360, no. 9348 (2002): 1892. 6. C. L. Drake et al., «Shift Work Sleep Disorder: Prevalence and Consequences beyond That of Symptomatic Day Workers», Sleep 27, no. 8 (2004): 1453—62. 7. A. Azzi et al., «Network Dynamics Mediate Circadian Clock Plasticity», Neuron 93, no. 2 (2017): 441—50. 8. A. Azzi et al., «Circadian Behavior Is Light-Reprogrammed by Plastic DNA Methylation», Nature Neuroscience 17, no. 3 (2014): 377—82.
9. C. J. Madrid-Navarro et al., «Disruption of Circadian Rhythms and Delirium, Sleep Impairment and Sepsis in Critically Ill Patients: Potential Therapeutic Implications for Increased Light-Dark Contrast and Melatonin Therapy in an ICU Environment», Current Pharmaceutical Design 21, no. 24 (2015): 3453—68.
10. S. Vásquez-Ruiz et al., «A Light/Dark Cycle in the NICU Accelerates Body Weight Gain and Shortens Time to Discharge in Preterm Infants», Early Human Development 90, no. 9 (2014): 535— 40.
11. K. Wulff et al., «Sleep and Circadian Rhythm Disruption in Psychiatric and Neurodegenerative Disease», Nature Reviews: Neuroscience 11, no. 8 (2010): 589—99.
12. L. Xie et al., «Sleep Drives Metabolite Clearance from the Adult Brain», Science 342, no. 6156 (2013): 373—77.
13. J. Mattis and A. Sehgal, «Circadian Rhythms, Sleep, and Disorders of Aging», Trends in Endocrinology and Metabolism 27, no. 4 (2016): 192–203.
14. J. E. Kang et al., «Amyloid-β Dynamics Are Regulated by Orexin and the Sleep-Wake Cycle», Science 326, no. 5955 (2009): 1005—7.
15. A. Di Meco, Y. B. Joshi, and D. Pratico, «Sleep Deprivation Impairs Memory, Tau Metabolism, and Synaptic Integrity of a Mouse Model of Alzheimer’s Disease with Plaques and Tangles», Neurobiology of Aging 35, no. 8 (2014): 1813—20.
16. J. Vienne et al., «Age-Related Reduction of Recovery Sleep and Arousal Threshold in Drosophila», Sleep 39, no. 8 (2016): 1613—24.
17. A. Chaix and S. Panda, «Ketone Bodies Signal Opportunistic Food-Seeking Activity», Trends in Endocrinology & Metabolism 27, no. 6 (2016): 350—52.
18. R. Chavan et al., «Liver-Derived Ketone Bodies Are Necessary for Food Anticipation», Nature Communications 7 (2016): article no. 10580.
19. M. P. Mattson, «Lifelong Brain Health Is a Lifelong Challenge: From Evolutionary Principles to Empirical Evidence», Ageing Research Reviews 20 (2015): 37–45.
20. H. B. Wang et al., «Time-Restricted Feeding Improves Circadian Dysfunction as Well as Motor Symptoms in the Q175 Mouse Model of Huntington’s Disease», eNeuro 5, no. 1 (2018): doi: 10.1523/ENEURO.0431-17.2017.
21. M. C. Yoon et al., «Treadmill Exercise Suppresses Nigrostriatal Dopaminergic Neuronal Loss in 6-Hydroxydopamine-Induced Parkinson’s Rats», Neuroscience Letters 423, no. 1 (2007): 12–17.
22. C. W. Cotman, N. C. Berchtold, and L. A. Christie, «Exercise Builds Brain Health: Key Roles of Growth Factor Cascades and Inflammation», Trends in Neurosciences 30, no. 9 (2007): 464—72.
23. A. J. Bruce-Keller et al., «Food Restriction Reduces Brain Damage and Improves Behavioral Outcome Following Excitotoxic and Metabolic Insults», Annals of Neurology 45, no. 1 (1999): 8—15.
24. M. L. Inder, M. T. Crowe, and R. Porter, «Effect of Transmeridian Travel and Jetlag on Mood Disorders: Evidence and Implications», Australian and New Zealand Journal of Psychiatry 50, no. 3 (2016): 220—27.
25. L. Yin et al., «Nuclear Receptor Rev-erbα Is a Critical Lithium-Sensitive Component of the Circadian Clock», Science 311, no. 5763 (2006): 1002—5.
26. Emily Manoogian, «A Prized Life: A Glimpse into the Life of Nobel Laureate, Dr. Roger Guillemin», myCircadianClock (blog), May 6, 2016, http://blog.mycircadianclock.org/a-prized-life-a-glimpse-into-the-life-of-nobel-laureate-dr-roger-guille min/.

